Breastfeeding and low blood sugar
There are two measures that should be introduced into routine hospital practices after birth and whose absence in the vast majority of hospitals is causing many mothers to stop breastfeeding even though they had originally intended to breastfeed.
First, babies should be skin to skin with their mothers as soon as possible after birth, not only premature babies but all babies. Even many babies who are showing signs of difficulty adjusting to the outside environment, especially these babies, often will improve their adaption if skin to skin with the mother. Skin to skin contact between the mother and baby should be considered both normal and also, a therapeutic measure and skin to skin contact be given the chance to help improve a baby’s adaptation to the outside environment. It is proven that a baby who is skin to skin with his mother maintains blood sugar levels better than a baby who is not or who is in an incubator. Skin to skin contact, without the baby being dressed, obviously, should be routine postpartum care for at least the first few hours after birth. Not only does the baby maintain his blood sugar better, but also, is much more stable with regard to his heart rate, respiratory rate and blood pressure.

Skin to skin contact immediately after birth helps maintain the newborn baby’s blood sugar and other functions. From Christensson K, Siles C, Morena L, Belaustequi A, de la Fuente P, Lagercrantz H, et al. Temperature, metabolic
adaptation and crying in healthy full-term newborns cared for skin-to-skin or in a cot
Acta Paediatr 1992;81:488–93
As well, skin to skin contact after birth provides an opportunity for babies to start breastfeeding and getting breastmilk from the breast soon after birth. Breastmilk is another way to help maintain blood sugar levels in the baby, much better than formula.
Secondly, mothers should be shown how to know whether their baby is getting breastmilk from the breast – that is to be able to tell whether the baby is drinking well or not. If the baby is drinking well, the mother should be re-assured; if the baby is not drinking well, then the first step to take is to improve the breastfeeding and help the baby get more milk from the breast.
Hypoglycemia (low blood sugar) is one of the commonest reasons for formula supplementation in the first few days after birth. Many babies are tested for low blood sugar for no good reason, and most babies get formula by bottle also unnecessarily.
1. Doing routine blood sugars on every baby at birth is another example of how “worrying about being sued” causes damage to babies and creates unnecessary anxiety in the parents and results in unnecessary “treatment”. Many hospitals in the US have this policy and more and more are adopting this policy in Canada. Interestingly, most pediatricians and neonatologists don’t seem to know what normal is. They look at a number and say, “give formula”.
2. In fact, nobody agrees on what is a normal blood sugar in newborns. Everyone has a different number they consider “too low”.
3. The blood sugar in babies is more or less the same as the mother’s blood sugar at birth and then over the next 1 to 2 hours the sugar drops, for some babies, into the range many would call “too low”. But this drop in the blood sugar is NORMAL! (see the graph). And the blood sugar rises again over the following hour or two even if the baby is not fed. This has been shown not only in humans but also in all mammals that have been studied. Treating “low blood sugar” in this circumstance is treating NORMAL and thousands of babies across North America are being unnecessarily supplemented with formula for what is a normal blood sugar.
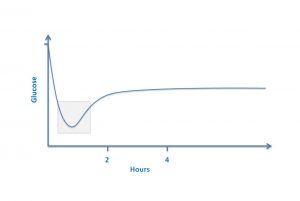
Normal glucose levels in normal newborns in the first hours after birth
Various physicians have become unnerved because the above graph does not contain units. That’s not the point. The point is that it is normal for the blood sugar to drop in the first hour or two after birth. You want graphs with numbers? Here is a study from 1986 and still after more than 30 years, many pediatricians don’t know about the drop. Here is another study from 2000. And here is an article from a world expert on the issue of hypoglycemia. What does Dr Jane Hawdon write in this article?
“Almost all babies have a sharp fall in blood glucose in hours after birth and then a slow rise from a nadir which occurs in the first 12 h… However as with other potentially precarious postnatal adaptations, there is a backup plan and the healthy baby responds to falls in blood glucose by mobilising and using alternative fuels to glucose. Thus, healthy babies are unlikely to manifest clinical signs or sustain brain injury during this physiological postnatal fall of blood glucose.”
4. Skin to skin contact with the mother maintains a higher blood sugar in the baby than separation of the mother and baby. Skin to skin contact also affords the baby an opportunity to feed at the breast.
5. The mother’s own colostrum is the best milk and banked breastmilk the second best to prevent and treat low blood sugar in newborn babies. This is because breastmilk does not stimulate the production of insulin in the baby as much as does formula. For this reason, we recommend that mothers whose babies are at high risk for low blood sugar express and store their milk starting at 35 to 36 weeks gestation so the baby, if necessary, can get colostrum instead of formula. There is no evidence that hand expression of milk at this stage increases the risk of premature birth. See the photo below that shows the amount of colostrum one mother expressed before the baby was born.

Prenatally hand-expressed colostrum by one mother
6. There is evidence that babies who are at risk for low blood sugar and are fed at the breast immediately after birth are less likely to become clinically hypoglycemic and actually have higher blood sugars than babies fed formula as their first feeding.
7. There is no evidence that a baby who is born big (some hospital policies say 4 kg=8lb 12oz or higher) is at risk for low blood sugar if his mother is not diabetic. On the contrary, such babies are at lower risk of hypoglycemia because they have lots of body fat that can be broken down into compounds called ketone bodies.
8. Ketone bodies protect the baby’s brain from the effects of low blood sugar and ketone bodies are present in much higher concentrations in the blood of babies breastfed (or fed colostrum or breastmilk) than in the blood of babies formula fed. Babies fed both breastmilk and formula have a lower but intermediate response.
9. There is no need for a baby at risk for low blood sugar (infants of diabetic mothers, both type 1 and type 2) to automatically go to special care. They should stay with the mother, skin to skin, be fed on demand and get help from the nursing staff to make sure the baby feeds well at the breast. Pre-expressed colostrum can be fed by spoon, syringe or lactation aid at the breast. See this article on mothers with gestational diabetes and this article on mothers with type 1 diabetes, where the authors felt that mothers and baby should be kept together and the babies not necessarily sent to special care. In the article on mothers with gestational diabetes, the authors write: “breastfed infants had a significantly higher mean blood glucose level compared to those who were formula fed for their first feed”.
10. Bottom line? There is a lot of hysteroglycemia out there and the “treatment” of it is causing many babies to be unnecessarily supplemented with formula often with bottles. In one case of a mother who contacted me, the baby was admitted to the NICU because an unnecessary blood sugar was done shortly after birth (during the time that the blood sugar sometimes NORMALLY drops to “hypoglycemic” levels.) The baby had an intravenous was given formula. The mother was feeding with a nipple shield (for reasons that did not seem clear, probably because the baby refused the breast after receiving bottles, but to me NO reason for nipple shield use is clear) and pumping her breasts. The baby was in the NICU for several days at great cost to the health system. All because of an unnecessary blood sugar being done as a “routine”. This baby had no risk factors for hypoglycemia. In another recent case, a baby whose mother had gestation diabetes was “ripped from her breast” as she said, so that the baby’s blood sugar could be measured. The baby was then transferred to NICU even though, apparently, the baby had been breastfeeding well.
If you need help with breastfeeding, make an appointment at our clinic.
Copyright: Jack Newman, MD, FRCPC, 2017, 2018, 2020

